As the COVID-19 pandemic has entered its second year, it continues to place unprecedented demand on health systems around the world. The NHS has been forced to adapt to this increased burden while also managing vaccination and booster rollouts. A resulting impact on patient experience is to be expected, however for the first time, using PEP Health’s Patient Experience dashboard, we can quantify this effect in real time – and use the insights to understand differences across whole populations, organisations, departments, and aspects of patient care.
The surge in confirmed COVID-19 cases in the last month, driven by the omicron variant, has led to repeated record daily case numbers. This has placed a dual burden on the NHS, as increased demand coincides with increased staff absences due to sickness. As a result, six trusts in England have been forced to declare “critical incidents”, as reported by the BMJ on Tuesday. Since then, at least 18 more trusts have followed suit, amounting to more than one in six across England. These pressures are particularly acute in certain "crunch points” such as A&E, which are disproportionately impacted by the increased patient volumes during winter.
Using our patient experience data, we can qualify and visualise this impact on care. To do this, we collect and analyse large volumes of public online patient feedback continuously collected across multiple online platforms, to provide a robust, representative, and up-to-date view of patient experience. These comments are analysed in real time using bespoke PEP Health technology and standardised methodology, to identify departments and a range of quality issues such as “fast access” and “effective treatment”. This enables hospitals to benchmark their patient experience to peer organisations.
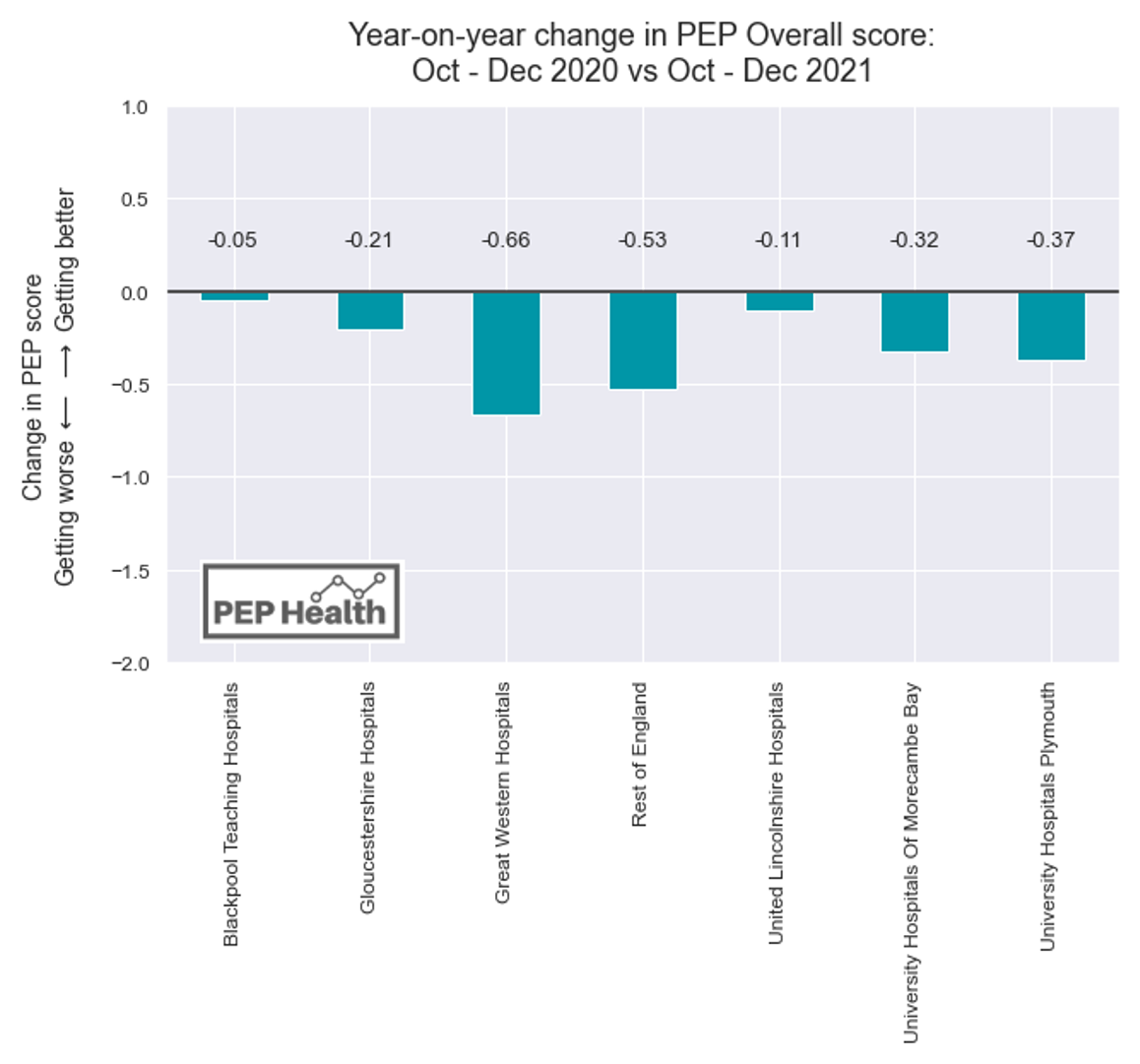
Figure 1 looks at the year-on-year change in overall score between the last 3 months of 2020, with the last 3 months of 2021. Results are shown for the six trusts that first declared a state of emergency, as well as the rest of England, and clearly reveal that all trusts are experiencing falls in patient experience.
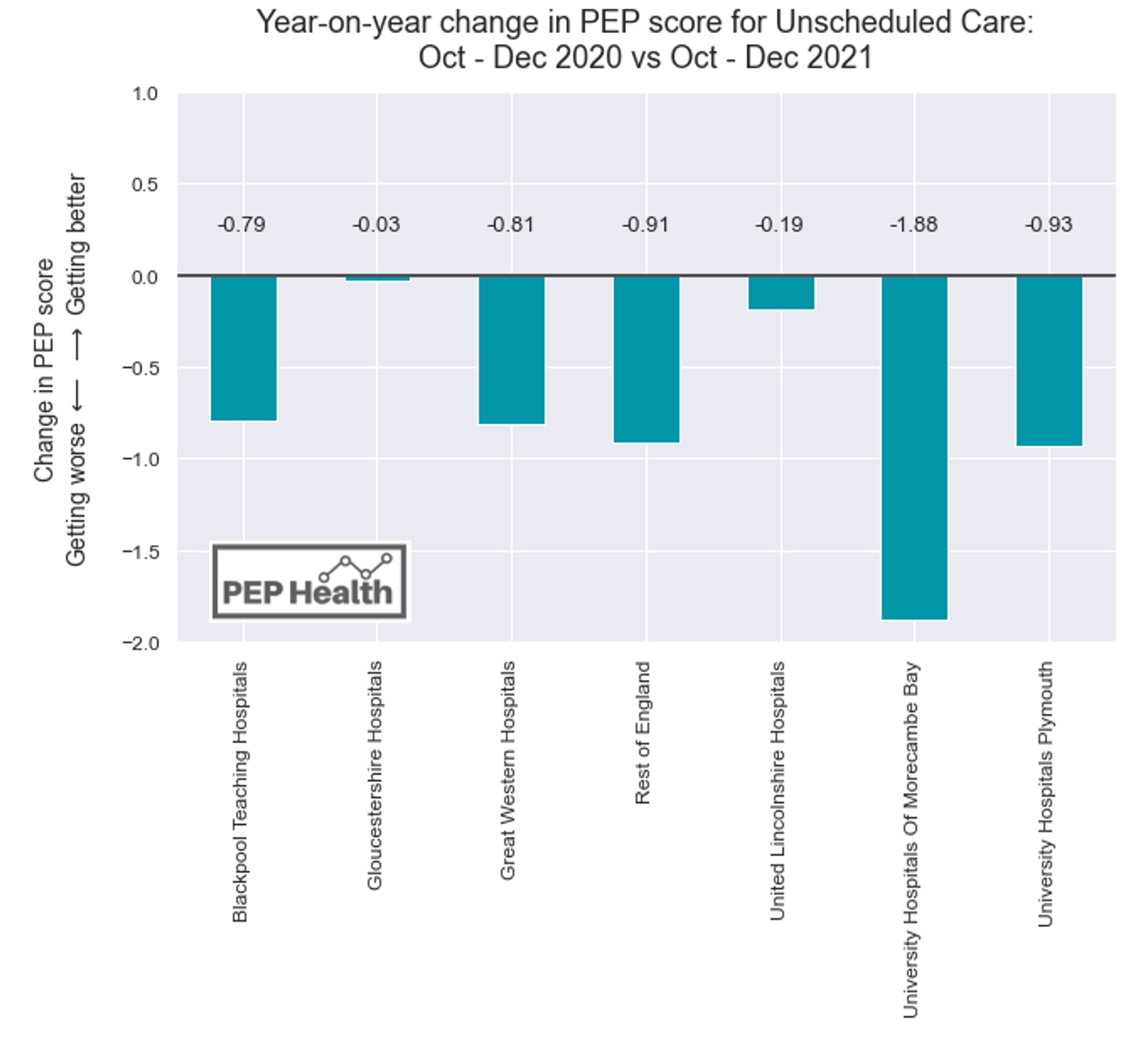
As discussed in our What Patients Think report, A&E performance is closely correlated with the overall performance of a trust. It can be seen as a “canary in the coalmine” – a powerful indicator of the trust’s overall resilience, that can predict if the wider organisation is struggling. Given that A&E is particularly affected by additional pressures from COVID-19, then patient experience here is a powerful barometer for the overall health of a trust.
Figure 2 then examines the change between the same periods as Figure 1, this time looking specifically at scores for Unscheduled Care, which covers A&E as well as minor injury units and walk-in clinics. We can see that again, the score has fallen for all six trusts, as well as the rest of England. Furthermore, in every case except Gloucestershire Hospitals, this decrease was greater than the drop in overall score. It is particularly striking that these drops in score are not isolated to the six trusts which have declared critical incidents. Rather than being outliers, this change in score is consistent in data from the rest of England. Patient experience is reflecting nationwide pressure on A&Es, and wider health systems – and warns that more trusts may be forced to declare a state of emergency while case levels continue to peak.
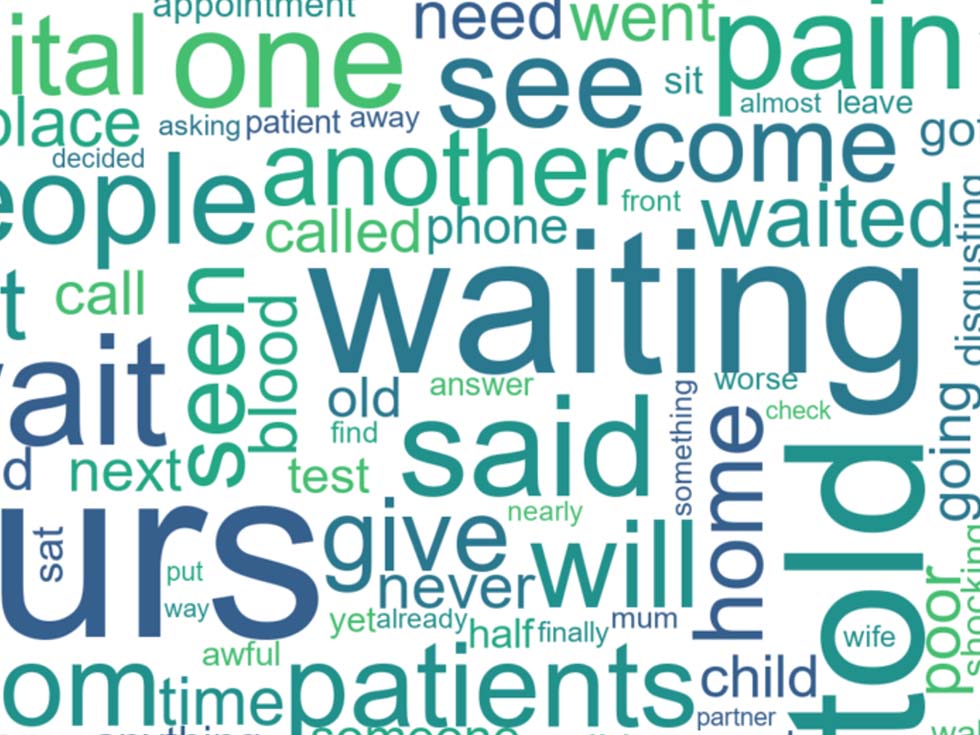
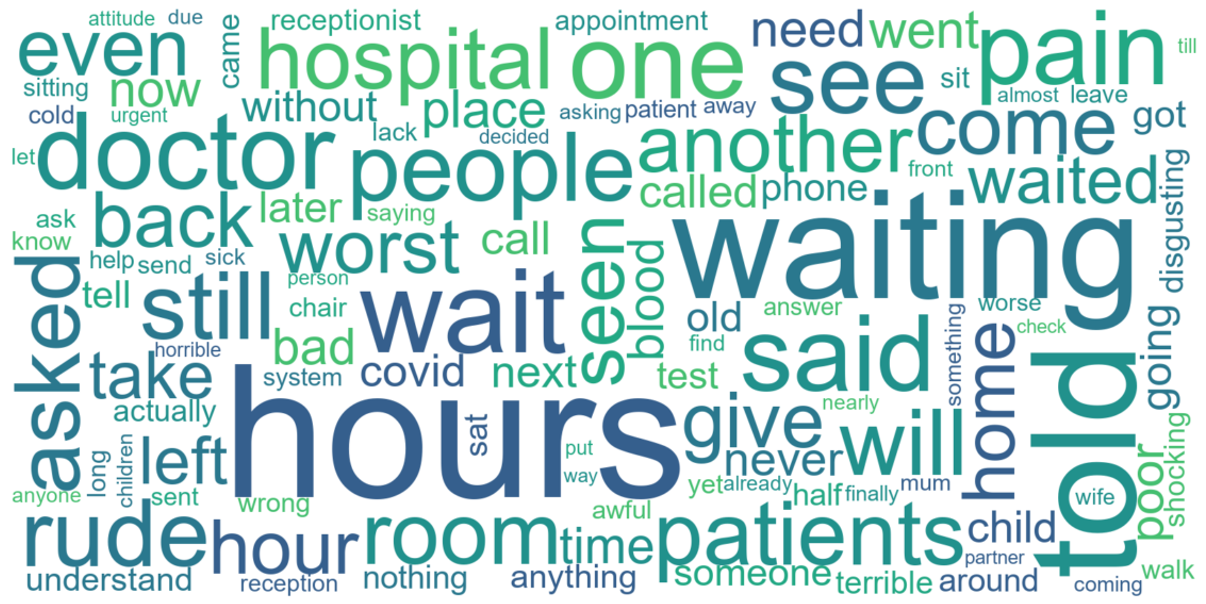
Utilising large volumes of data allows us to understand patient experience from both a qualitative and quantitative perspective. We can dig deeper into the specific topics which resonate with patients. Figure 3 shows key words from positive comments, while Figure 4 contains key words from negative comments – both based on A&E reviews in England since October 2021. We can see that the negative comments focus on wait times, with “wait”, “waiting” and “hours” appearing frequently, alongside terms relating to communication such as “told”, “asked” and “rude”. However, the positive comments nonetheless demonstrate appreciation and gratitude for the care that has been received – with “thank”, “care” and “staff” standing out, along with positive adjectives – “amazing”, “caring”, “friendly” and “excellent”.

Our client partnerships are using PEP to better understand their patient experience, identify areas of improvement to focus on, and boost staff morale. If you would like to know how your A&E unit is performing and which aspects of care need to improve from the point of view of your patients, please contact enquiries@pephealth.ai.