Maternity care in England continues to be associated with avoidable harm, resulting in cases of serious disability, psychological trauma and substantial burdens on the health system, including the significant costs associated with litigation. Identifying variation from the National Mean in a near real time way could provide unique insight into emerging safety issues and declining performance, enabling Trusts, the regulator, ICS’s and the system to benefit from actionable insight to drive quality improvement.
Our custom platform PEP Health uses real-time patient insights derived from over 10 million comments a year including traditional survey sources and digital sources such as publicly available social media posts and online forums to identify best practice, measure variations in care and drive timely improvements in care. We offer NHS Trusts the chance to monitor their patient experience in a contemporaneous and in-depth way, identifying how patients perceive their experience of care but also enabling Trusts to identify key variations in care and emerging safety issues.
Every comment is scored 1 (worst) to 5 (best). The overall score for a review is usually given by the user alongside their comment. Where that’s not the case, for example with tweets, we have developed a custom model trained on the millions of user-scored comments we have to automatically score it for us with a high degree of accuracy. Our models are also able to identify the department(s)/service(s) discussed by the user – or derive them for where they have made their comment – to track not only specific aspects of care, but where that care takes place.
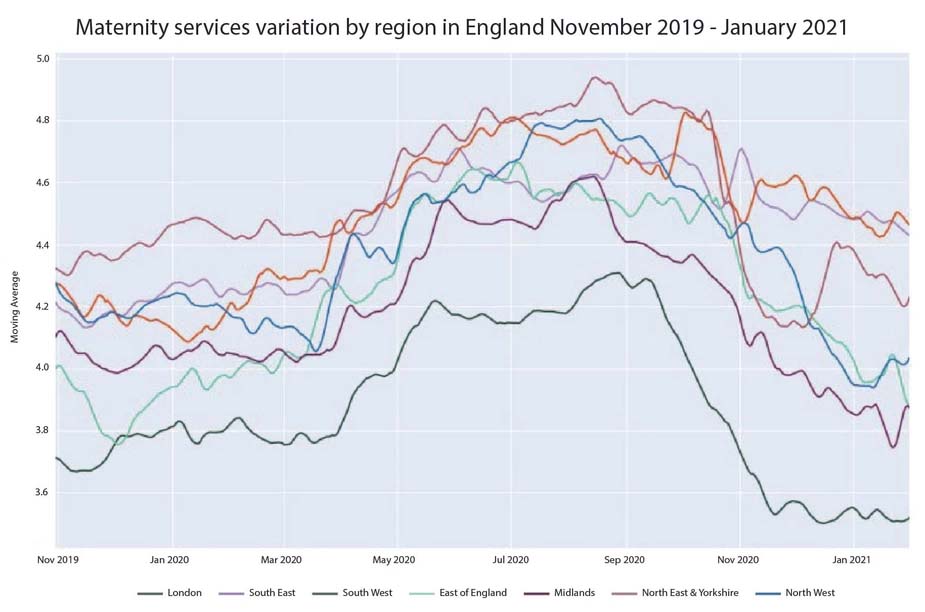
In fact, current analysis by PEP health has identified that significant variations in the patient experience of maternity services exists across England.
There are three key observations that this figure highlights; that all maternity services found the recent lockdown posed many challenges to maintaining their standard of service provision, that variation has widened over the last year and lastly, that those Trusts who were already struggling to cope pre-COVID have deteriorated the most.
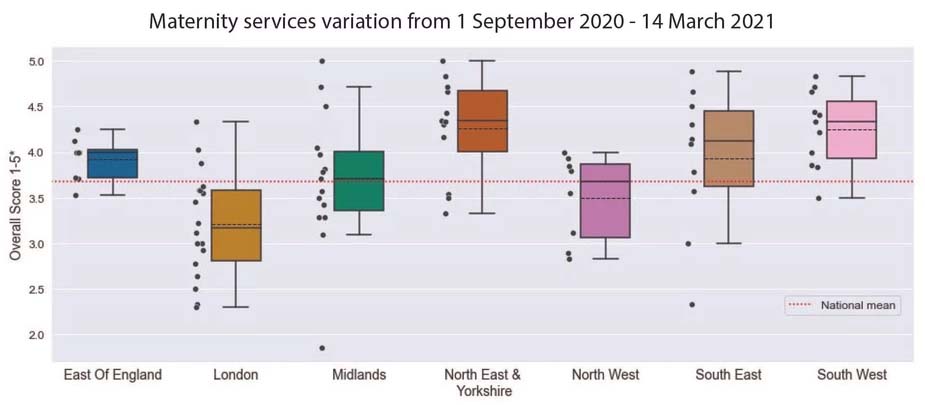
Unpacking these findings further, PEP Health can identify the individual Trusts within the regions, highlighting where Trusts aggregated patient experience scores are well below the National Mean, and in some cases at a near critical level.
Each black dot on the graph represents a Trust within the associated region. Here we can see that there are a number of Trusts, most notably in Midlands, South East and London that are preforming significantly below the National Mean. The outputs of our analysis could be used in various unique ways, to encourage proactive engagement with the underperforming Trusts to support them with local network improvements, to work in cooperation with the regulator to prioritize inspections, or to promote the Trusts to work together and support shared learning across the network. With the recent announcement that NHS England will commit nearly £100M to improve maternity safety in England, our data could be used to help prioritize investment and evaluate improvement programs.
In fact, as the recommendations in the recent Ockenden report are considered these insights would support two of the immediate and essential actions outlined in the report: to enhance the Trusts ability to actively listen to patients and to encourage peer-to-peer support and review of care.
Looking to the Future
Better listening to patients has been identified in repeated enquiry findings as an essential step to improve the quality of care delivered. Understanding where and why we
have such wide variation in service provision would help not just users but the whole system to improve. The consequences of dealing faster with these underlying issues would not only accelerate improvements but with the real-time visibility ongoing it would help them stick too.
By listening to and measuring all maternity units across the nation we could potentially find the next “inadequate” rated unit before the CQC inspection even happens and at the same time help reduce the 5% of all patients that receive some form of avoidable harm whilst in hospitals and the associated litigation and remedial costs. Our next blog will investigate how failures in the maternity services at specific Trusts could have been predicted through the patient experience platform and we will give our recommendations on how the insights from real time patient feedback can help Trusts make the essential improvements necessary to avoid future failure.
In the meantime, if you would like to know how your maternity unit is performing from the point of view of your patients, please contact: enquiries@pephealth.ai
