Overview
From 2020-2021, as part of a Cancer Improvement Collaborative, PEP Health worked with NHS England, 25 Cancer Alliances and 12 participating NHS trusts to help investigate and improve the experiences of people with Rare and Less Common Cancers (RLCC). The Cancer Collaborative is a network of shared learning between these 25 Cancer Alliances whose aim is to lead the way in healthcare service improvement. A core objective of the NHS Cancer Plan is to improve patient experience for people living with and accessing cancer services across the health system.
NHS England wanted to accelerate evidence-based service improvement to reduce unnecessary delays for patients, contribute towards the delivery of cancer waiting times targets, enhance patient’s experience of care and improve the working lives of staff. They commissioned PEP Health to provide additional intelligence to inform and guide future work for the NHS Cancer Programme. The data insights team at NHS England recognised that social media could provide valuable insights into the care received by RLCC patients which could be shared among the Cancer Improvement Collaborative.
The current method of patient feedback
Feedback is traditionally collected through the annual Cancer Patient Experience Survey (CPES), which is part of the NHS Cancer Programme. However, the patient insights team recognised that there were some key gaps in the survey methodology. These included a lack of data around palliative care experience, long lag times between collecting the data and generating insights, as well as declining response rates during the COVID-19 pandemic.
It was felt that by exploring alternative datasets, such as digital and online feedback, they could develop a set of insights on cancer pathway patient experience. The aim was to add value and create data triangulation opportunities for local improvement teams to feed into their intervention and improvement strategies.
The solution
Using sophisticated machine learning and engineering, PEP Health gather millions of patient comments across multiple online platforms for all NHS trusts in England. Natural language processing algorithms are applied in three specific ways to automatically generate insights from the high volume of text based comments. The models collect and clean the data, sentiment analyse and score each relevant comment, and then theme the comment by care principles such as effective treatment, emotional support, and fast access .
The analysis conducted for this project used this method and compared all comments against cancer specific and rare and less common cancer comments to generate a unique insight into the variation in patient experience that exists across the cancer services.
Results
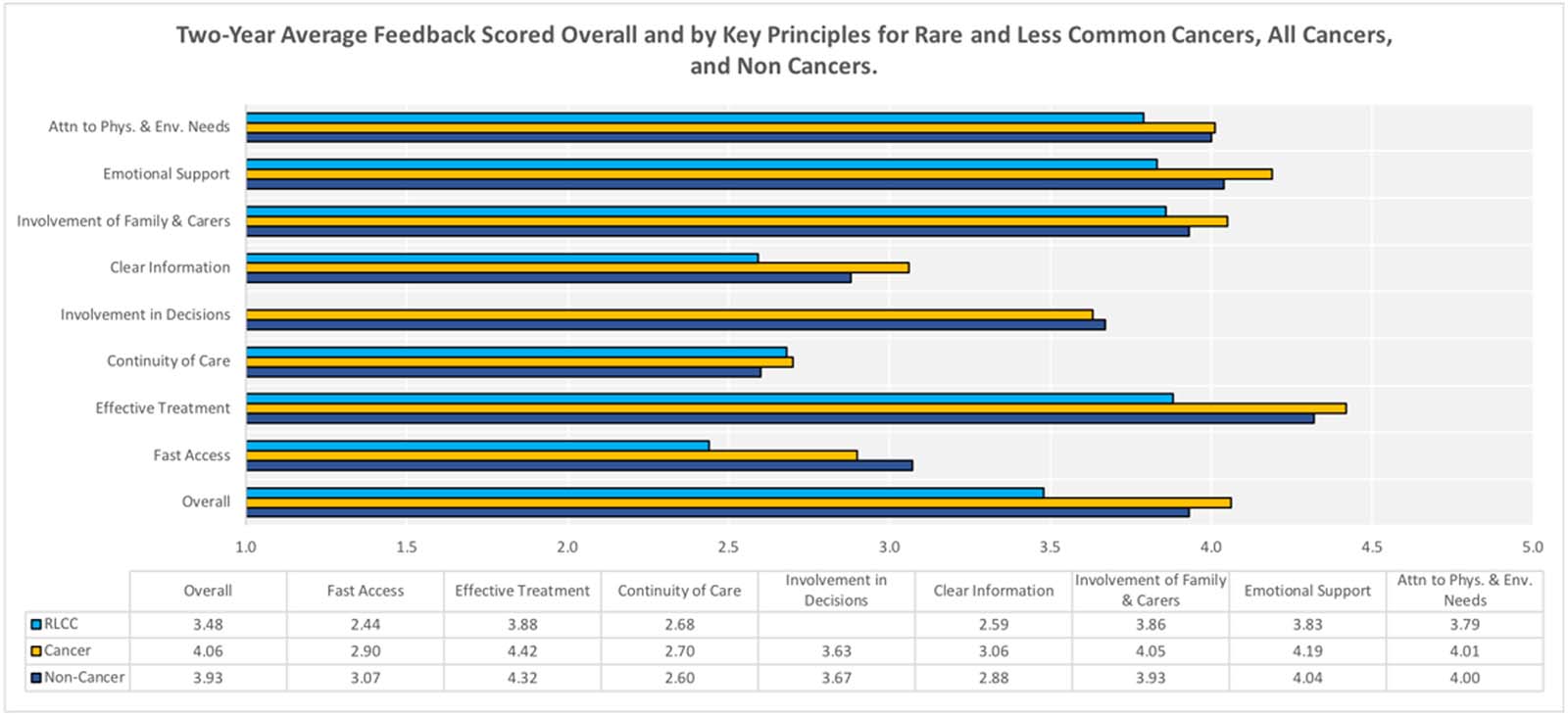
Overall, the PEP Health analysis revealed a positive picture, with cancer related comments scoring higher for patient experience than all other comments. It showed that cancer patients tend to comment on effective treatment, emotional support, and fast access to care more often than other care principles. There were also some important key differences found including:
- Comments from those with rare and less common cancers were less positive on fast access compared to all other cancer and non-cancer comments
- Overall scores as well as emotional support and fast access scores had decreased across the board, (for RLCC, Cancer and Non-Cancer)
- Effective treatment and emotional support score highest for in-patient experience, while continuity of care and clear information score lowest
- RLCC patient comments report poorer experiences across all domains compared to those for Non-Cancer and Cancer patients, apart from continuity of care (as shown in the graph below).
How did it help the cancer collaborative at NHS England?
Using social media insight and finding a new data source to understand the current picture in the cancer pathway helped NHS England to pinpoint areas for improvement. Using these data sets NHS trusts were able to see in real time what improvements needed to be made. PEP Health were able to identify differences in experience for certain cancers such as kidney, skin and blood, which allowed NHS England to see where changes might need to be made in these pathways and allocate resource accordingly.
PEP Health’s innovative, standardised methodology for analysing patient feedback is the first of its kind. Using evidence-based results has the potential to bring meaningful improvements to patient care, quality and staff experience.
The Cancer Alliances used the insight from this work to inform their recovery plans from COVID-19 including the work they were asked to do as part of personalised stratified follow up pathways. NHS England can now use the data collected during this study to help other trusts to create improvement strategies which are more informed by the broader context of patient experience. It will enable them to focus resource where it is most needed for patients in a holistic way – viewing the insight in multiple contexts, rather than seeing it as one pathway for all cancers.
What’s next?
Having an accurate understanding of how services are changing is a fundamental step in achieving replicable and sustainable quality improvement. The ambition is to share and spread this work further to continue to generate insight and better NHS England’s understanding of what the NHS and the people who use it need.
This methodology could also be used for other disease conditions. For example, PEP Health’s empirical evidence has just been published by the Lancet, describing the variation in patient experience of those living with obesity or who are overweight across different regions in England.
Feedback
This work is real innovation on the edge with the potential to bring about great and meaningful improvements to patient care and staff experience through the power of words. Never before has digital data from social media been used in this way for NHS cancer services and it is encouraging that the outputs from this work show exciting potential to improve our understanding of what people say. If we are able to find a way to scale up these methodologies, their machine learning algorithms could be game changing for NHS providers. Claire Enston
Head of Insight and Feedback at NHS England
PEP Health is helping us to better understand and listen to what patients think and what matters to them in their own experience of cancer services. We aim to increase qualitative feedback to balance our transformation initiatives, evaluate what’s working through the patient’s own voice, and to ensure that our actions are best aligned to earlier and faster diagnosis which leads to greater personalised care for each individual patient’s needs. Michael Ryan
Head of Cancer Alliance - East Midlands, NHS England and NHS Improvement
1 The eight care principles include; 1. fast access to reliable health advice 2. clear information, communication and support for self-care, 3. effective treatment delivered by trusted professionals, 4. emotional support, empathy and respect, 5. continuity of care and smooth transitions, 6. involvement of, and support for family and carers, 7. involvement in decisions and respect for preferences, 8. attention to physical and environmental needs.